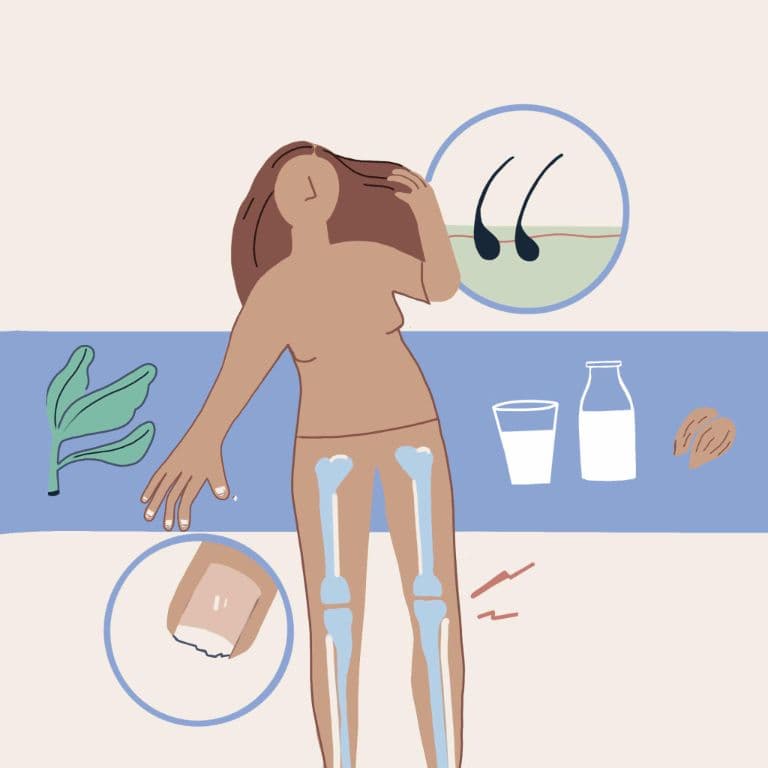
Osteoporosis is a lifelong condition wherein there is a progressive reduction of bone mass, thus making the bones weak and prone to frequent fractures. Menopause and osteoporosis are directly linked.
In women, the hormone estrogen is responsible for healthy bones. Estrogen keeps the bone density intact and prevents the bones from becoming weak. But after a woman reaches menopause, her estrogen levels start declining rapidly. Naturally, this imbalance of hormones in the body affects bone health too - they lose calcium and start becoming weak, fragile and porous.
At what age you would develop osteoporosis depends on your bone mineral density. But generally, after 35 years of age, the bone mass starts declining at a rate of approximately 0.4% in women. During menopause, the rate of losing bone mass rises to 2-5% for the first 5-10 years. Women who attain early menopause - which can be due to many different reasons - are at a higher risk of getting affected with osteoporosis.
Even though osteoporosis is not curable, there are many ways to manage it to prevent fractures and slow down its further development. If these preventive measures are not followed at an early stage, it can worsen osteoporosis. Some symptoms of severe osteoporosis can be fractures with trivial trauma, severe back pain, curved back, loss of height and a hunched posture.
Here are 11 ways you can manage your osteoporosis
Prevent falls
Since osteoporosis comes with a risk of fractures, one of the most important ways to manage the condition is to prevent falling or slipping. For this purpose, several modifications in the space you live in or where you spend the most amount of time can help.
- Reduce the clutter in the space to reduce the risk of bumping into anything and falling.
- Keep minimal furniture to make your place more spacious to move around easily.
- Install non-slippery tiles in your rooms and bathrooms.
- Use rugs with a non-skid backing.
- Keep night lamps on so that you can make your way in the dark as well.
- Use anti-skid footwear when going outdoors.
Wear padded protectors
Hip fractures are the most common type of fractures that can occur during osteoporosis. To protect yourself, you can wear hip protectors which are padded devices that help in reducing the intensity of the impact if you happen to fall.
Increase your calcium intake
Calcium is the most vital mineral for healthy bones and teeth. If you have osteoporosis, you need at least 1000-1200 mg of calcium daily or as per your doctor’s advice. Animal-based calcium-rich foods include non-fat milk, low-fat yoghurt, and salmon. Plant-based calcium-rich foods include plant-based milk like soy milk, orange juices fortified with calcium, broccoli, cauliflower, tofu, dark green leafy vegetables, sesame seeds, amaranth seeds, amaranth leaves.
If you are not able to meet your daily recommended calcium requirements, your doctor may also suggest calcium supplements.
Include Vitamin D in your diet
Calcium is not of much use to the body without the intake of Vitamin D that helps in the effective absorption of calcium in the body. Calcium supplements already have some amount of Vitamin D in them. The best source of Vitamin D is sunlight. It is good to go for morning walks or sit under the sunlight. Food sources to gain Vitamin D include egg yolks, mushrooms and deep marine fish.
Avoid high-phosphorus foods
Too much phosphorus in the blood makes the body extract calcium from the bones to balance the blood in the body. So if you have osteoporosis, it is better to avoid phosphorus-rich foods as too much of it can increase bone loss. High-phosphorus foods include red meats, soft drinks, and foods with phosphate food additives.
Exercise regularly
Exercising is necessary for everyone, especially if you have bone disorders. A sedentary lifestyle and inactivity can further weaken your bones. Exercising for 30-45 minutes daily or at least three times a week can strengthen your bones and muscles, preventing you from reaching a severe level of osteoporosis. Daily exercise will also boost your confidence; the strength you gain can prevent you from falling.
You can do a combination of various exercises:
●Aerobic exercises
●Resistance training
●Walking
●Running
●Sports like tennis
●Dancing
●Climbing stairs
●Weightlifting
However, always take your doctor’s advice to understand which form of exercise is best suited for your condition.
Hormonal replacement therapy
During and after menopause, women become estrogen-deficient and is one of the primary causes of bone loss in menopausal women. Hormonal Replacement Therapy is one of the treatments for preserving Bone Mineral Density (BMD). Estrogen supplements are available in the form of oral tablets, vaginal cream, gel or a patch based on your convenience.
Natural remedies
Phytoestrogens are plant-derived compounds showing similarities to the female sex hormone, estrogen. Natural alternatives containing phytoestrogens for treating osteoporosis include:
●Soy products
●Red clover
●Flaxseed or flaxseed oil
●Dong Quai - Chinese herbal medicine
●Black cohosh
Please do consult your doctor before consuming any of these.
Quit smoking, alcohol and caffeine
Tobacco, alcohol and caffeine make our body’s pH acidic. For a balance between alkalinity and acidity, the body extracts calcium from the bones, necessary for crucial body functions like heart and muscle contractions. It can further weaken the bones and make them more brittle, increasing the risk of fractures.
Undergo regular screening for bone density
Lastly, if you are in the postmenopausal stage, you should get your Bone Mineral Density tested at least once every year. Since there are no direct symptoms of osteoporosis, you must visit a doctor whenever you experience back pain or any other bone-related pain in other body parts to prevent fractures.