This blog is compiled by Athira Krishnan, a content writer for Proactive For Her.
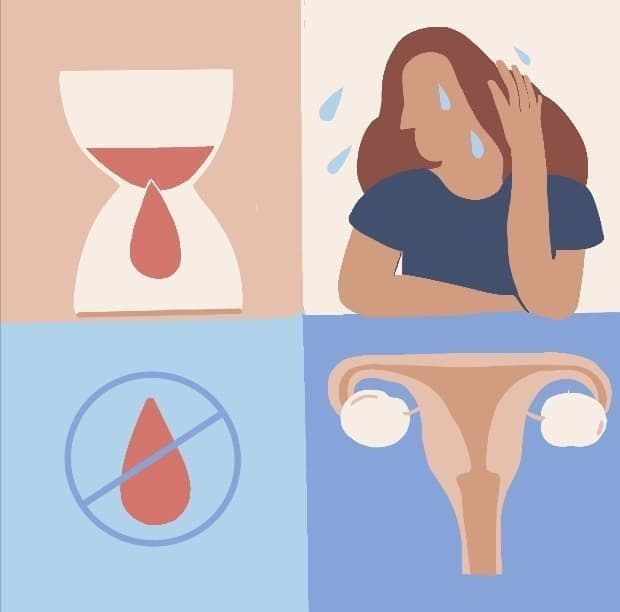
What is perimenopause and menopause?
Perimenopause is the period in which the ovaries gradually begin to produce less estrogen. It usually starts in women’s 40's but can start in their 30’s or even earlier. Perimenopause lasts up until menopause, the point when the ovaries stop releasing eggs and thereby, stop menstruating. Menopause marks the end of female reproduction
How to recognize abnormal vaginal bleeding during periods?
Normal period cycles last from 21 to 45 days. If your cycle occurs lesser or more than this time period, or when the bleeding is heavier (more than 80ml a day) or lesser ( less than 5ml a day ) than usual, or if your period persists for a longer time period, i.e, longer than 4-7 days, you may have abnormal vaginal bleeding.
What could be the causes?
- Hormonal imbalance - This is a common occurrence during the perimenopausal and menopausal periods. As women age, usually after 40 years, the optimum functioning of the ovaries gradually reduces and this change causes the balance between the hormones estrogen and progesterone to shift. This is what causes hormonal imbalance. PCOD (Polycystic Ovarian Disease) and Thyroid are conditions that develop due to this.
- Endometrial hyperplasia -The endometrium is the lining of the uterus and becomes thick because of hyperplasia (having too many cells). During the perimenopausal stage, the thickness of the inner lining should be between 5-15 mm. If it is thicker than 15 mm, it can cause abnormal vaginal bleeding. This extra thickening occurs when estrogen hormone levels are high.
- Abnormal mass in the uterus - Uterine fibroids are abnormal swellings in the uterus that usually appear during childbearing years and are non-cancerous
Uterine polyps are growths attached to the inner wall of the uterus and are majorly non-cancerous. These abnormal growths occur due to increased estrogen levels.
- Adenomyosis of the uterus - Adenomyosis is a condition in which the inner lining of the uterus (the endometrium) breaks through the muscle wall of the uterus (the myometrium) in which one of the symptoms is abnormal vaginal bleeding during the period. Menstruators often experience extremely painful periods in adenomyosis as well.
- Infections in the uterus and the cervix can cause abnormal bleeding.
- Congenital bleeding disorders that affect the coagulability quality of the blood causes this condition.
- Excess weight gain/sudden weight loss - This leads to hormonal imbalance, which then may lead to abnormal bleeding.
- Cancers of the uterus, cervix or ovaries - These cancers usually develop post menopausal age.
- Certain contraceptives - Some side effects of usage of contraceptive pills, IUD’s (Intrauterine Devices) that are inserted into the uterus may include abnormal vaginal bleeding.
- Certain medications - Blood-thinning medication used to treat other conditions and antidepressant medication may also contribute to abnormal bleeding.
- Stress- Emotional and physical stress
- Dysfunctional uterine bleeding - When there is abnormal vaginal bleeding with no discernible or specific cause, it is called dysfunctional uterine bleeding.
What are some symptoms you could experience?
- Changes in the regular cycles of your period are characterized by excessive or reduced bleeding as compared to normal.
- Pain that wasn’t observed in previous regular cycles.
- In cases of infections, there may be foul-smelling white discharge mixed with blood
- During normal menstrual flow, there is usually no presence of clots. But women who have irregular bleeding might present with clots.
- Feeling of indigestion, constipation, excessive flatulence may occur due to hormonal imbalance.
How is this condition diagnosed?
Your doctor may suggest one or more of these tests help you understand the cause of this bleeding.
- Routine blood test: First, you might be asked to get your blood work done. In the blood-work, the haemoglobin count is checked for anaemia and clotting factors are looked into to check for any congenital blood disorders
- Hormones: The levels of the hormones estrogen, progesterone and thyroid are checked along with the masculinizing hormones or androgens. Your doctor may also ask you to have prolactin checked.
- If the doctor has any concern to suspect a pregnancy, they would advise, a pregnancy test to rule out pregnancy or a recent abortion.
- Ultrasonography of the pelvis is done to check for any mass in the ovaries, uterus or cervix.
- Some advanced tests like hysteroscopy are recommended in certain cases where a scope with a camera is slowly inserted into the uterus through the vagina to check for any growths or swellings in the interior of your vagina, cervix, uterus or tube. In some other cases, a biopsy (a sample of tissue taken from the body in order to examine it more closely) may be taken.
- If ultrasound doesn’t prove to be conclusive, then your doctor is likely to suggest an advanced form of imaging such as an MRI.
How can this be treated?
- Managing with medication alone- This is where only medications are prescribed to the patient to reduce/remove symptoms. In the initial form of treatment, your gynaecologist may recommend you to try this treatment for 3-6 months before exploring other methods.
- Hormone treatment - Since hormonal imbalance is one of the major causes of abnormal bleeding, the patient is recommended a hormone treatment plan. The prescribed hormone pills have to be taken every day for 3-6 months after which the doctor revisits your medication with you in a follow-up visit. Most women usually respond well to this treatment and the symptoms are usually relieved.
- Tranexamic acid -If you have mild symptoms, your doctor may recommend tranexamic acid that helps in the quick clotting of the blood to prevent excessive bleeding.
- Gonadotropin-releasing hormone (GnRH) - In women struggling with fibroids, cysts and polyps, doctors might suggest medicines called as GnRH analogues. This is also a cyclical treatment and the drug has to be taken daily for 3-6 months.
- Desmopressin - This drug is prescribed for patients with blood coagulation disorders.
- Hormonal IUD - This device is inserted into the uterus and releases some amount of the progesterone hormone regularly, every day for those who don’t respond to oral medication. The devices have a lifespan of 5-10 years after which they have to be removed/replaced.
- Surgery - If you don’t see any relief from these symptoms, it may be worthwhile considering some surgical options.
- Endometrial ablation - This minor procedure removes the inner lining of the uterine wall. Most women are relieved of symptoms with this procedure.
- Myomectomy & Polypectomy - Myomectomy is the removal of fibroids and Polypectomy, the removal of polyps from the uterus.
- Hysterectomy - When the above mentioned minor procedures don’t work, hysterectomy (removal of the uterus) is turned to as a last resort. In rare cases, the ovaries and fallopian tubes are also removed along with the uterus.
- Uterine Artery Embolization - If one doesn’t want their uterus removed, this procedure can be performed, in which the blood supply to the uterus is blocked and abnormal vaginal bleeding naturally stops.
- Cancers - For cancers of the female reproductive system, surgery, radiation and chemotherapy are the procedures done depending on what type of cancer is present.
What could be some side effects/complications of the treatment procedures?
For the hormone treatments: One could experience side effects such as acne, bloating of the stomach, swelling and hair loss. For the hormonal IUD: One could experience side effects such as some amount of pain, more than usual vaginal white discharge and in rare cases, infection.
What could be some complications that could arise from abnormal vaginal bleeding?
If untreated, you might lose a lot of blood and hence can lead to anaemia. Anaemia can cause fatigue and palpitations. If untreated, anaemics also have an increased risk of heart failure and infections. If masses in the uterus/cervix are left untreated for a long period of time, high-risk masses could have a chance of cancerous change.
What are some preventive measures that you could take?
Regular pap smear is advised for women after 40 years. In cases where there is a family history of cancer, an annual check-up can be done. If not, it can be done every 2 years.
- Regular screening with Mammography and ultrasonography is advised to rule out breast and ovarian cancer.
- In young girls who just attained menarche, a vaccine called HPV is recommended. This prevents cervical cancer to a significant extent. It is advised to get this vaccine done as early as possible post menarche.
- Most importantly, maintain a stress-free lifestyle. This will, to a great extent prevent undue hormonal imbalances, thus greatly preventing the chances of abnormal vaginal bleeding.
Conclusion
Abnormal bleeding is observed more and more in recent times due to our lifestyle changes and high levels of stress. The major cause of such bleeding is hormonal imbalance. Stress is one of the key factors that induce these hormonal imbalances. Practising a stress-free, healthy and physically active lifestyle early on reduces the chances of developing this condition later, during the perimenopausal and menopausal period.
Disclaimer- This information is provided for educational purposes and should not be construed as medical advice. Please consult with your healthcare practitioners before undertaking any changes in your diet or adding supplements.
Proactive For Her is a digital clinic for women, offering accessible, personalized, and confidential health-care solutions. We offer products and services for out-patient health concerns of Indian women, across their lifetime - from puberty to pregnancy to menopause. To know more on the sexual and reproductive health of women, visit https://www.proactiveforher.com/