It is possible that in recent casual conversations with women, you’ve heard the term ‘PCOS’ being used. This term is either understood superficially amongst those in the conversation or if someone asks for clarification; more often than not, the answer is stuttered back to the group using keywords like cysts on the ovaries, irregular periods, acne, weight gain, etc. It is evident that the person who is answering, and their acquaintances have neither wholly understood the process, nor are they too convinced about the seriousness of this issue. This, however, is normal- a product of the lack of conversation about a condition that is becoming rapidly commonplace, in urban and liberal spaces.
Reading up on already established research and explanations given by reputed medical sources has often rendered me thoroughly overwhelmed regarding this condition’s sheer complexity that involves so many crucial body processes. I found it incredibly difficult to process, relate to and comprehend. All of this, a struggle I am indeed not alone in, further adds to the pre-existing haze and uncertainty surrounding PCOS.
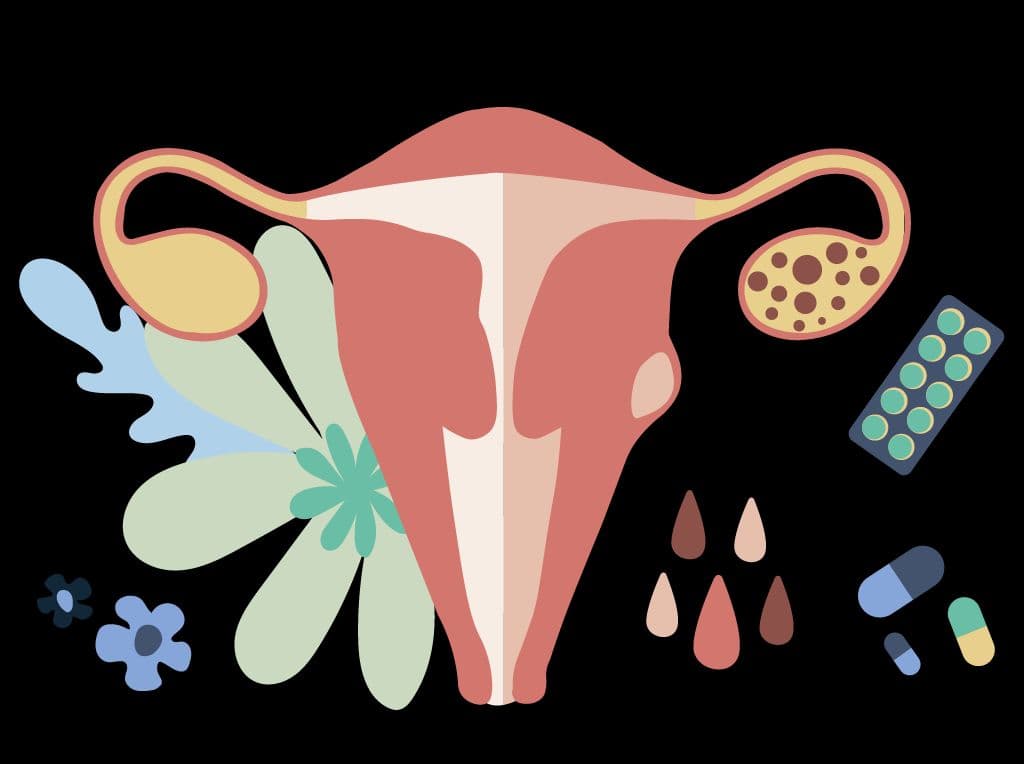
Rather than a specific ‘disease’ ( which is a word often misattributed to PCOS), Polycystic Ovarian Syndrome (PCOS) is considered by many experts to be a ‘constellation of symptoms’. The causes of these symptoms are not 100% clear or understood. However, it is obvious that this is one of the most common hormonal problems experienced by young women in the world today. A quick mnemonic device that’s helped me in explaining and understanding the main characteristics of PCOS is ‘CIA’-
- C-Cysts (in the ovaries)
- I- Irregularity (in periods)
- A- Androgens (heightened levels of male hormones)
To truly understand what goes awry in a woman diagnosed with PCOS, it is essential to understand what a ‘normal’ menstrual cycle looks like. It involves a complex series of interactions involving the brain and its hypothalamus and pituitary gland. Both are crucial components of the body’s endocrine system and are responsible for creating and transmitting hormones in the body. From the hypothalamus, a hormone termed as ‘GnRH’ is released, which stimulates the pituitary gland to release two essential hormones that trigger the process of ovulation and menstruation in the female body.
These hormones- the FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone) then travel from the brain to the ovaries via the bloodstream, triggering the ovaries to release an egg which then travels to the uterus. If fertilised by the sperm (i.e. the male reproductive cell that enters the female body in the event of sex), this egg stays in the uterus. Still, if not, it is shed along with the endometrium (the inner lining of the uterus) – resulting in a woman having her period.
So what goes wrong for someone who has been diagnosed with PCOS? The issue begins with the first step in the process- irregularities in the release of GnRH in the brain, which then impacts FSH and LH levels that are released. One of the main repercussions of this imbalance is that the ovaries now make more androgens- i.e. testosterone (the hormone related to masculinity) in the female body. While the necessary female hormones that aid the menstrual and ovulation process are lacking -ultimately resulting in an inhibition of the crucial sequence of events that cause one to menstruate. Due to these reasons, one diagnosed with PCOS has irregular periods, heightened levels of androgens and some, even experience infertility due to the unhealthy eggs produced by the ovaries as a repercussion of the cysts and hormonal imbalances.
It is at this point that I would explicitly like to state that living with PCOS is hard. I am not a trained medical health professional, just a young woman who has lived with PCOS for the past four years. As mentioned before, reading medical information, similar to the one offered above, can be a source of anxiety and confusion. In defining the process in technical terms, we often strip off the subjective, lived and real experiences and feelings that many women diagnosed with PCOS go through. PCOS harms the mental well being of women and also has sociocultural implications. Particularly hard hit are young women (who are a large component of diagnosed cases) who live in a society with set standards of femininity and what a female body should look like. Although the processes involved in triggering PCOS might be internal, its repercussions manifest on features of the body. So, what often initiates visits to the gynaecologist’s office is women experiencing apparent irregularities in the functioning of their menstrual cycles and bodily features.
In my case, I began to miss my monthly period, to an extent where I went five months without one. When my period did arrive, I’d be in extreme pain, clutching the sides of my abdomen with a hot water bag on my lower back. All of this was accompanied by severe nausea and exhaustion. I also noticed an increase in pimples and whiteheads on my face, an increase in hair fall- one stroke of the brush would pull out multiple strands of my hair. I also gradually noticed a fat layer surrounding my abdomen that wasn’t present in my childhood years. My body was covered with hair- no amount of waxing was enough. There was an increase in small brown spots all over my stomach and hair on my chest. I also wondered why the back of my neck and underarms were darker than the rest of my body- no amount of my mother’s skincare and whitening cures seemed to work.
I think it’s essential for us to acknowledge the impact these changes have on our feelings when are bodies transform from being recognisable to something now considered alien. I remember being filled with an extreme loathing for my body and being particularly hard on myself because I didn’t look like other girls in magazines or the ones near me. Things that further intensified these negative feelings were conversations with my peers, particularly with those from different cultures than my own.

I used to be an international level sportsperson. I had teammates from all over India and Maharashtra (the state I live in) hailing from regions that were not particularly vocal about the female body’s issues. When I was first diagnosed, I remember telling my teammates about the issue because it very prominently affected my ability to play the game. Those who understood the gist of what I said explained it to the others in hushed tones. The word ‘hormone’ was told in a very derogatory manner, and I remember all of them looking back at me critically because of the ‘sexual’ connotation attached to my condition. This is representative of what many people diagnosed with PCOS go through, be it with their family members, peers and immediate society, and the number of people they have to converse with to get help. We are very often shamed and taught to internalise the blame attributed to the development of this disorder- by healthcare professionals, parents, and other crucial figures in our lives. It is this same punishment that we exercise on ourselves as we look in the mirror in frustration. No matter how hard we try, our weight just doesn’t reduce. We still get acne, are hairy and have to spend loads of money to rectify these bodily aberrations to pass off as conventional females in our society.
Something that aggravated my internal struggle was my lack of access (in these early stages of my interaction with PCOS) to a clear, credible and concise explanation of my condition. My experience with the diagnosis process left me flustered. I was told simply to lose 20 kilograms, after a quick check at the weighing scale and prescribed hormone medications that I dutifully consumed despite experiencing their adverse side effects. I visited many professionals, and in all these 7-minute interactions, the causes, impact and consequences of my diagnosed condition were left unexplained. I completely understand that doctors may not have the time to get into in-depth lessons on the female body, mainly when there is a waiting room full of patients with several other complicated ailments. Yet, who do we turn to if not for the experts in the field? Suppose the answer lies in school and college educators. In that case, the unfortunate reality of the situation, in my experience, is that the general conservatism of Indian society regarding topics labelled as ‘sexual’ seep into the textbooks and our teachers’ lesson plans as well. I recall my biology teacher completely glossing over the topic of sex and menstruation in my private, national board school. This experience immediately caused me to ponder the state of affairs regarding ‘sex education’ in municipal or state-run schools?
This ultimately brings us to the socio-cultural impact and divide of having PCOS, particularly in societies with an ambivalent relationship with any topics related to the female sexual body. For many, the day a young girl gets her first period is celebrated because she is now of reproductive age and can finally contribute to her future role as a woman by becoming a mother. After this, Indian women go through variations of how they are treated during their ‘time of the month’. It’s a topic hidden from male household members; pads are covered with newspaper from the shop to their disposal; women are shunned out of specific duties and spaces in the household, and into their rooms. How, then, do women who face complications with this already dicey area cope with their immediate society’s pressures and attitudes?
Research suggests that women from urban spaces are more likely to develop PCOS than those from rural areas. Many attribute this disorder to a luxurious and sedentary lifestyle complete with stress which causes the body to react in this manner. This further amplifies the self-blaming cycle most women diagnosed subject themselves to. As stated at the beginning of this article, the causes in developing PCOS are not clear. Various other uncontrollable factors, such as one’s genetics also impact the development of this disorder.
The need of the hour is evident. Most women go through their journey with PCOS alone, particularly in communities that silence all discussions about women’s bodies. Speaking up and sharing our stories is step one in remedying the lack of conversation on this issue. The next essential step is to build a community of people like us, who support, educate and motivate each other inclusively in coming to terms with our condition, working together to get and feel better. We’ve begun. Let’s embark and face the hurdles coming our way on this journey, together.
Disclaimer - This information is educational and should not be construed as medical advice. Please consult your doctor before making any dietary changes or adding supplements.
ProactiveForHer is a digital clinic for women, offering accessible, personalised, and confidential healthcare solutions. We offer out-patient care, diagnostic services and programs for various health concerns of Indian women, across their lifetime - from puberty to pregnancy to menopause. To know more on the sexual and reproductive health of women, visit https://www.proactiveforher.com/