I’ve often heard myself and other women use the apology- “I’m sorry, I’m on my period”- to explain certain behaviours that might be considered uncharacteristic or ‘irrational’ by those around us. Although women might use the apology jokingly in specific contexts, it reveals a very real phenomenon that many women experience when they’re on their period. There is a reason why most period tracking apps we use also have a separate section attributed to tracking our emotions. This is because there is a clear correlation between our period and our low moods when we are menstruating.
“I’m PMSing right now” is another phrase we hear. Premenstrual syndrome, premenstrual dysphoric disorder and premenstrual exacerbation are severe conditions that impact one’s mood, especially in the week or so before their periods. Common moods experienced are- heightened feelings of anger, irritability, anxiety and sadness that might manifest in crying and increased sensitivity. This is what women with ‘normal’ menstrual cycles experience. What then happens to women with PCOS who have irregular periods and frequent hormonal fluctuations?
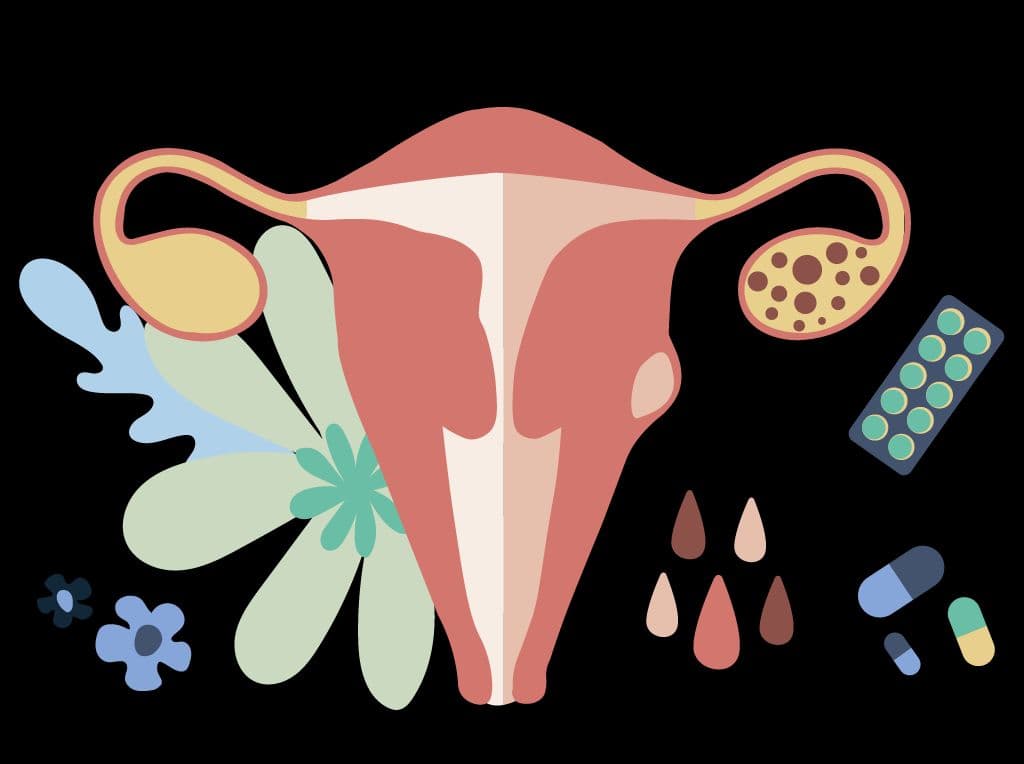
PCOS is a serious medical condition experienced by a staggeringly large number of young women. It is characterised by cysts on the ovaries, irregular periods, heightened androgen levels in the female body, and a plethora of other symptoms. The primary hormones involved in a female’s reproductive cycle are estrogen and progesterone. Fluctuations in both adversely influence the serotonin levels- an essential neurotransmitter that regulates moods, sleep cycles and one’s appetite.
Let’s break this down. When we speak of moods- we refer to one’s feelings or their state of mind at any particular time. Everyone experiences different types of moods- positive or negative. In the context of menstruation, low moods that give rise to negative emotions are a dominant feature. However, mood disorders are less common and are intense and long-lasting mental states that can impair one’s ability to function ‘normally’. Most widely known mood disorders are depression and bipolar disorder. Mood disorders, anxiety, somatic and eating disorders are highly prevalent in persons struggling with PCOS.
Medical health researchers and practitioners are yet to establish a strict cause and effect relationship between PCOS and mental disorders. However, most researchers adopt multiple legitimate hypotheses and prevalence rates that state a clear relation between both variables. Some state a connection between insulin resistance and sex hormone imbalances– notably higher levels of androgens (common symptoms for those with PCOS), that affect the secretion of certain hormones leading to side effects of prolonged stress and depression in the individual. Researchers have noticed through their studies that women with PCOS markedly report lower neurotransmitter levels- serotonin, which, as stated earlier, are instrumental in regulating one’s moods.
The above neurobiological symptoms are not the sole contributor to the comorbidity of PCOS and mental illnesses. While hormonal and neurotransmitter imbalances worsen one’s mental well-being, they do not negate or supersede other contributors to the development of mental illnesses such as past traumatic experiences, insecurities, fears, socio-economic conditions and other phenomena that lead to illnesses such as depression and anxiety.

In addition, the perception of one’s body and prevailing cultural standards of beauty also has an impact on our mental health. PCOS physically manifests as acne, dark spots and patches, weight gain, and excessive hair growth both on the body and the face. These are considered deviations from what the ideal female body is supposed to look like. Women are constantly expected to conform to the standard of fair, unblemished skin with luscious hair and a slender frame. The reality of the situation is that women with PCOS do not meet most of these standards. This can culminate to extreme body dysphoria, low self-esteem, low confidence and a hatred for one’s body and ultimately one’s self- all of which heavily contribute to or can be the source of one’s deepest fears and despair. Prescribed medication to treat both the woman’s physical and mental condition can also increase all of the above physical reactions to the disorders.
Being diagnosed with a chronic illness such as diabetes, high blood pressure, or even PCOS is a significant stressor in women’s lives and impacts physical and emotional and mental health. Many societies and cultures also expect women to procreate and fulfil their obligations of providing children to their families. This can be a source of immense emotional and physical stress for the woman in question, particularly if they fail to meet this societal expectation and are shamed for the same. Some women may have to undergo medical treatment that corrects the levels of certain hormones that are secreted, all of which have physical and mental side effects. This lonely journey is filled with stress, anxiety, pressure, disappointment and frustration.
My journey is also rife with the above circumstances. I was 16 when I was first diagnosed with PCOS and 19 when I was diagnosed with clinical depression and anxiety. When the psychiatrist asked me when I first started feeling this way prominently, I drew the parallel between my PCOS journey and my mental health journey. I am in no way stating that PCOS was the sole cause of my mental illness. However, I am bringing light to the correlating timelines- where fluctuating neurobiological mechanisms could have increased the intensity of my low mental state and helped me recognise that this was when my mental condition markedly became worse and began to impair my ability to function. Medication for both these conditions has also affected my weight, acne, appetite, sleep and menstrual cycle.
Well-meaning people immediately offer us solutions to both conditions, which are predominantly medication, exercise and diet. However, many don’t understand that mentally ill individuals experience extremely low levels of motivation and lose interest or the capability to engage with even the most basic daily activities. Therefore, it is challenging for exhausted individuals with low energy levels and motivation to partake in these activities. And so this unfortunate, seemingly punishing cycle continues.
There is a dire lack of conversation on this issue because these are two stigmatised topics, particularly in the Indian framework. The Indian woman’s journey and sexual or reproductive experiences are often lonely, something personal that she must deal with secretly. With no one to talk to about this very physical manifestation of PCOS diagnosis accompanied by severe changes in one’s mental wellbeing can be an alarming phenomenon to experience alone. It is essential then for us as women to build a healthy support system amongst ourselves. A support group that encourages women to share their stories and develop joint, realistic strategies in tackling their conditions.
Furthermore, we should check up on each other’s progress non-judgmentally and help one another through both the highs and lows that are a part of our collective journeys. Living with PCOS is a tough reality to bear alone. So let’s do our best to be there for each other with empathy, kindness and unconditional support.
Disclaimer : This information is educational and should not be construed as medical advice. Please consult your doctor before making any dietary changes or adding supplements.
ProactiveForHer is a digital clinic for women, offering accessible, personalised, and confidential healthcare solutions. We offer out-patient care, diagnostic services and programs for various health concerns of Indian women, across their lifetime - from puberty to pregnancy to menopause. To know more on the sexual and reproductive health of women, visit https://www.proactiveforher.com/